
Burns

Dr. Takshak Deshmukh Plastic Surgeon ( प्लास्टिक सर्जन )
Read MoreDr. Tanaya Deshmukh Gynaecologist ( प्रसुती व स्त्रीरोग तज्ञ )
Read More
Burns
Scar revision

Skin Grafting

Cleft lip/palate
Hand Surgeries
Gynecomastia

Vascular anomalies

Ear anomalies

Diabetes Foot Ulcer

Pressure Sores
Liposuction

Abdominoplasty
Fat Grafting
Breast Implants
Breast Reconstruction
Breast Reduction

Split Ear Lobule

Treatment of post wound healing
Pre-Pregnancy Checkup & Treatment
Normal Delivery

Caesarean Section

Painless Normal Delivery
Laparoscopic Tubectomy
Laparoscopic Hysterectomy
Diagnostic Lap-Hysteroscopy
Vaginal Hysterectomy
Infertility Treatment
Uterine Cancer Diagnosis and Treatment
Sonography facility available
N.S.T. facility available

Burns are a common injury that can range from mild to severe and often leave lasting scars or marks on the skin. These marks, especially from second and third-degree burns, can be permanent if not treated properly. However, with the right care and treatment, burn marks can be reduced or minimized. Below is some essential information about burns and how to reduce their scars.
For severe burns, it’s essential to consult with a healthcare professional or dermatologist for the best treatment options, which may include:
. Skin Grafts: For large third-degree burns, a doctor may recommend a skin graft to replace the damaged skin with healthy skin from another part of the body.
. Scar Revision Surgery: In some cases, cosmetic surgery can be done to improve the appearance of the scar, although this is usually considered when the scar is severe or affects the person’s mobility.
Scar revision is a type of surgery used to improve the appearance of scars. Scars are a natural part of the body’s healing process, but in some cases, they may become raised, pitted, or discolored, requiring medical intervention. Scar revision procedures aim to flatten, smooth, and reduce the visibility of scars.
Scar revision surgery can include the following options:
. Laser Treatments: To improve skin texture and appearance.
. Surgical Excision: Removing the scar tissue and re-stitching the skin.

Skin grafting is a surgical procedure in which skin is taken from one area of the body (donor site) and transplanted to another area (recipient site) to repair damaged or missing skin. It is commonly used for treating severe burns, chronic wounds, or skin defects. Skin grafting helps restore the appearance and function of the skin and reduces scarring.
There are different types of skin grafts depending on the severity of the injury:
.Split-thickness graft : Only part of the skin is removed, including the epidermis and part of the dermis.
.Full-thickness graft : The entire thickness of the skin is removed from the donor site.

A cleft lip and/or cleft palate is a birth defect that causes a gap or opening in the upper lip and/or the roof of the mouth (palate). This condition can occur on one or both sides of the face and may be present in varying degrees of severity. A cleft lip can be present with or without a cleft palate.
Surgery is typically performed to repair the cleft lip and/or palate. The goal is to restore function and improve the appearance of the lip and/or palate. Surgery may include:
.Cleft Lip Repair : This surgery is usually performed when the baby is around 3 to 6 months old.
.Cleft Palate Repair : This surgery is typically done when the child is around 9 to 18 months old.
Additional surgeries may be necessary as the child grows to address speech, dental, or other issues that arise.
Hand surgery refers to procedures used to treat various conditions affecting the hand, wrist, or forearm. It may be necessary due to injuries, congenital defects, arthritis, or other conditions that limit the function of the hand. Depending on the condition, surgery may be performed to restore mobility, reduce pain, or improve the appearance of the hand.
.Carpal Tunnel Release Surgery: Performed to relieve pressure on the median nerve in the wrist, helping to reduce symptoms of carpal tunnel syndrome.
.Tendon Repairs: Necessary when tendons in the hand or wrist are damaged, often from injuries or conditions like rheumatoid arthritis.
.Fracture Repair: If bones in the hand or fingers are broken, surgery may be needed to align and stabilize the bones for proper healing.
.Joint Replacement: In cases of arthritis, joints in the fingers, wrist, or thumb may need to be replaced with artificial implants.
.Reconstructive Surgery: This may involve rebuilding parts of the hand that have been severely damaged due to trauma, such as burns or accidents.
After hand surgery, patients typically undergo physical therapy to regain strength, flexibility, and function. Full recovery can take weeks to months, depending on the procedure and the individual’s condition.
It's essential to follow post-surgery care instructions closely to minimize complications and speed up recovery. Regular follow-ups with a healthcare provider ensure the success of the surgery and that the hand heals correctly.
Gynecomastia is a condition where males experience the enlargement of breast tissue. It can occur due to hormonal imbalances, weight gain, certain medications, or underlying health conditions. While it is common during puberty, it can also affect older men or those with obesity.
.Hormonal Imbalances: Changes in the balance of estrogen and testosterone, often during puberty or aging.
.Medications: Some drugs, including steroids, anti-androgens, and certain antidepressants, can lead to gynecomastia.
.Obesity: Excess fat can increase estrogen levels and cause breast tissue enlargement.
.Underlying Health Conditions: Conditions like liver disease, hyperthyroidism, or kidney failure can contribute to gynecomastia.
Treatment depends on the severity of the condition and its underlying cause. Options include:
.Medications: In some cases, medication may be prescribed to adjust hormone levels and reduce breast tissue growth.
.Surgery: For persistent or severe cases, surgical intervention, such as liposuction or mastectomy (removal of breast tissue), may be required.
After surgery, patients may need to wear a compression garment to support the chest. Full recovery can take several weeks, with normal activities resuming after a period of rest and healing. Pain is typically manageable with prescribed medications.
It's important to follow post-operative care instructions, and follow-up appointments with the doctor are essential to ensure proper healing.

Vascular anomalies refer to abnormal growths or malformations in the blood vessels. They can occur anywhere in the body and may be present at birth or develop later in life. These anomalies are typically categorized into two main types: **vascular tumors** and **vascular malformations**.
.Hemangiomas : These are benign tumors made up of abnormal clusters of blood vessels. They are common in infants and can appear as red or purple spots on the skin. Most hemangiomas shrink over time, but some may require treatment.
.Arteriovenous Malformations (AVMs) : These are abnormal connections between arteries and veins that bypass the capillary system. AVMs can occur in any part of the body and may cause pain, swelling, or bleeding. They are usually more serious and may require surgical intervention.
.Venous Malformations : These involve abnormal growth of veins and may cause pain, swelling, and blood clots. Treatment may include sclerotherapy (injection of a substance that causes the veins to close) or surgical removal.
.Lymphatic Malformations : Abnormal growths in the lymphatic vessels, often resulting in cyst-like masses, which can cause swelling and discomfort.
Treatment depends on the type, location, and severity of the vascular anomaly. Options include:
.Medications : Certain medications may be prescribed to shrink vascular tumors or manage symptoms, especially for hemangiomas and venous malformations.
.Sclerotherapy : For venous malformations or some AVMs, a substance is injected to close off the abnormal blood vessels.
.Laser Treatment : For surface-level hemangiomas, laser therapy can be used to reduce their appearance and prevent complications.
.Surgery : In cases where the anomaly causes severe complications, surgical removal of the abnormal blood vessels may be necessary.
Recovery after treatment depends on the type of vascular anomaly and the chosen procedure. For most cases, post-treatment care includes managing pain, swelling, and avoiding trauma to the treated area. Follow-up appointments are crucial to ensure that the anomaly has been adequately treated and that no further issues arise.

Ear anomalies refer to any abnormal development or structural condition of the ear. These can be congenital (present at birth) or acquired over time. Such anomalies can affect the outer ear (pinna), middle ear, or inner ear, leading to hearing loss, discomfort, or cosmetic concerns.
.Microtia: A congenital condition where the external ear (pinna) is underdeveloped or missing. Microtia can range from a mild deformity to complete absence of the ear.
.Anotia: A more severe form of microtia, where there is a complete absence of the external ear. It may be associated with hearing loss.
.Atresia: This condition refers to the absence or closure of the ear canal, leading to conductive hearing loss. It often occurs alongside microtia.
.Preauricular Tags: Small skin growths or mounds located near the ear, often linked with other ear anomalies. These are usually benign but may require removal if causing discomfort or for cosmetic reasons.
.Ear Deformities (Cup Shaped or Sticked Ear): Sometimes, the ear may have an abnormal shape or be abnormally positioned, such as in the case of "bat ear" where the ear sticks out excessively.
Treatment for ear anomalies depends on the type and severity of the condition. Some common treatment options include:
.Surgical Reconstruction (Otoplasty): In cases of microtia or other ear deformities, reconstructive surgery can be performed to reshape the ear. Otoplasty is often done to improve cosmetic appearance and restore normal ear function.
.Ear Canal Reconstruction: For individuals with atresia, reconstructive surgery can be performed to create a functional ear canal, allowing for hearing restoration.
.Hearing Aids and Implants: In cases where hearing loss is present due to ear anomalies, hearing aids or bone-anchored hearing implants (BAHA) can help amplify sound and restore hearing.
.Preauricular Tag Removal: If a preauricular tag is causing discomfort or for cosmetic reasons, it can be removed through minor surgical procedures.
After surgical treatment for ear anomalies, patients typically require some time to heal. Recovery time will vary depending on the specific procedure, but for most, it involves follow-up appointments to ensure proper healing and monitor any potential complications.
Children with ear anomalies may need ongoing care to monitor hearing and speech development, and early intervention is essential to improve long-term outcomes.

A diabetic foot ulcer is a serious complication of diabetes that occurs when a wound or sore on the foot fails to heal properly. These ulcers often develop as a result of poor circulation, nerve damage (neuropathy), and high blood sugar levels, which can impair the body's ability to fight infection and heal wounds.
.Neuropathy: High blood sugar can cause nerve damage, leading to numbness or reduced sensation in the feet. Without the ability to feel pain or discomfort, individuals may not notice cuts, blisters, or sores developing on their feet.
.Poor Circulation: Diabetes can damage blood vessels, reducing blood flow to the feet. This impaired circulation can slow the healing process and make it harder for the body to fight infections.
.Infection: When the skin is broken, bacteria can enter and cause infection. Since diabetes weakens the immune system, infections are more difficult to control and heal.
.Foot Deformities: Foot deformities like bunions, hammertoes, and calluses can increase the risk of developing pressure points and sores on the feet.
.Open sores or wounds on the foot, often on the bottom or toes
.Redness, swelling, or warmth around the wound area
.Pain or tenderness, although in some cases, numbness may occur due to neuropathy
.Discharge or drainage from the ulcer, often with a foul smell, indicating infection
.Changes in skin color around the ulcer, like darkening or a yellowish appearance
Treatment for diabetic foot ulcers aims to promote healing, prevent infection, and reduce the risk of complications. Common treatment options include:
.Wound Care: Regular cleaning and dressing of the ulcer to promote healing and prevent infection. The wound may be debrided (removal of dead tissue) to improve healing.
.Antibiotics: If the ulcer is infected, antibiotics may be prescribed to treat the infection and prevent it from spreading.
.Pressure Offloading: Reducing pressure on the ulcer by using special footwear, braces, or casts to prevent further irritation and promote healing.
.Blood Sugar Control: Tight control of blood sugar levels is essential in managing and preventing diabetic foot ulcers. Keeping blood glucose levels within a target range helps the body heal more effectively. .Surgical Intervention: In severe cases where the ulcer has not healed or the infection has spread, surgery may be required to remove infected tissue or even amputate the affected area to prevent further complications.
Preventing diabetic foot ulcers is crucial, and involves:
.Regular Foot Inspections: Check feet daily for sores, cuts, blisters, or other abnormalities. Seek medical advice if any issues arise.
.Proper Foot Hygiene: Wash feet daily with warm water and mild soap. Dry feet thoroughly, especially between the toes, to avoid fungal infections.
.Proper Footwear: Wear shoes that fit properly and avoid walking barefoot to reduce the risk of injury.
.Control Blood Sugar Levels: Keep blood glucose levels in check through diet, exercise, and medication as prescribed by a healthcare provider.
If you have diabetes and notice any signs of a foot ulcer, seek medical attention promptly. Early intervention can prevent serious complications, including infection and the need for amputation.

A pressure sore (also known as a pressure ulcer, bedsore, or decubitus ulcer) is a localized injury to the skin and underlying tissue, usually over a bony prominence, as a result of prolonged pressure, friction, or shear. Pressure sores commonly occur in individuals who have limited mobility, especially those who are bedridden or in a wheelchair.
.Prolonged Pressure : Continuous pressure on the skin reduces blood flow to the affected area, leading to tissue damage.
.Friction : When the skin rubs against clothing or bedding, it can lead to abrasions, increasing the risk of pressure sores.
.Shear : Shear occurs when layers of skin move in opposite directions, such as when a person slides down in bed. This can damage blood vessels and tissues.
.Moisture : Excessive moisture, such as from sweating or incontinence, can soften the skin, making it more prone to injury and infection.
.Redness and irritation : In the early stages, the skin may appear red, irritated, or inflamed, especially over areas of bony prominences.
.Pain : A pressure sore may cause pain or tenderness, depending on its severity and location.
.Blisters : As the pressure ulcer worsens, blisters, sores, or open wounds may appear.
.Skin Breakdown : Advanced pressure sores can result in deep wounds, often with exposed muscle, bone, or tendons.
Pressure sores are classified into four stages based on the depth of tissue damage:
.Stage 1 : Redness of the skin that does not fade with pressure relief. The skin may feel warm, firm, or swollen.
.Stage 2 : Partial thickness loss of skin, including blistering or an open ulcer.
.Stage 3 : Full thickness loss of skin, with damage extending to the underlying tissue. Fat may be visible in the wound.
.Stage 4 : Extensive damage involving muscle, bone, or tendons. There may be significant tissue loss, and the ulcer may be deep and wide.
Treatment for pressure sores focuses on relieving pressure, promoting healing, preventing infection, and managing pain. The main components of treatment include:
.Pressure Relief: Relieving pressure from the affected area is the most important step. This can be done by repositioning the patient regularly and using pressure-relieving devices such as special cushions, mattresses, or pads.
.Wound Care: Keeping the wound clean and properly dressed is essential to prevent infection and promote healing. The type of dressing depends on the stage and severity of the ulcer.
.Infection Control: If the pressure sore is infected, antibiotics may be required. Regular monitoring is crucial to identify and treat infections early.
.Surgical Intervention: In severe cases, surgery may be necessary to remove damaged tissue or repair the wound. Skin grafts may be used for large ulcers.
Preventing pressure sores is key, particularly in individuals who are at high risk. Key strategies include:
.Regular Repositioning: Change positions frequently to relieve pressure on vulnerable areas. For bedridden patients, repositioning every 2 hours is recommended.
.Use of Pressure-Relieving Devices: Specialized mattresses, cushions, and padding can reduce the pressure on the skin.
.Good Nutrition: Ensure adequate nutrition, including protein, vitamins, and minerals, to support tissue health and repair.
.Skin Care: Keep the skin clean and dry, and moisturize to prevent dryness or cracking that could lead to further damage.
.Inspect Skin Regularly: Check for early signs of pressure sores, especially in areas like heels, hips, elbows, and the lower back.
Seek medical advice if you notice any signs of a pressure sore, such as redness, irritation, or open wounds. Early treatment can prevent the ulcer from becoming more severe and reduce the risk of complications such as infection or tissue death.
Liposuction is a cosmetic surgery procedure designed to remove excess fat from specific areas of the body, such as the abdomen, thighs, arms, neck, and buttocks. This procedure can help contour and sculpt the body by targeting fat that is resistant to diet and exercise. Liposuction is not a weight-loss solution, but rather a body-shaping procedure for individuals near their ideal weight.
During liposuction, a surgeon makes small incisions near the target area and inserts a thin tube called a cannula. The cannula is used to break up and suction out fat cells. The procedure is typically performed under local or general anesthesia, depending on the extent of the treatment area.
.Tumescent Liposuction : The most common type, where a saline solution is injected to make the fat easier to remove.
.Ultrasound-Assisted Liposuction (UAL) : Uses ultrasonic waves to break down fat before suctioning it out.
.Laser-Assisted Liposuction (SmartLipo) : Uses laser energy to melt fat before it is suctioned out.
.Power-Assisted Liposuction (PAL) : A motorized cannula vibrates, making fat removal quicker and more efficient.
.Improves body contours and shape.
.Removes stubborn fat that doesn’t respond to diet and exercise.
.Can enhance self-esteem and body image.
.Produces long-lasting results when a healthy lifestyle is maintained.
While liposuction is generally safe, it carries certain risks, including:
.Infection
.Excessive bleeding or fluid loss
.Skin irregularities, lumps, or asymmetry
.Burns or nerve damage (in the case of ultrasound or laser-assisted methods)
.Anesthesia risks
After the procedure, patients typically experience swelling, bruising, and discomfort, which can last for several days. Most individuals can return to normal activities within a few days to a week, but strenuous exercise should be avoided for several weeks. Compression garments may be worn to help reduce swelling and support the healing process.
Ideal candidates for liposuction are individuals who:
.Are at or near their ideal body weight
.Have good skin elasticity
.Have localized fat deposits that are resistant to diet and exercise
.Are in good overall health and have realistic expectations for the procedure
If you're considering liposuction, it’s essential to consult a board-certified plastic surgeon who can assess your goals, review the risks and benefits, and help determine if you're a good candidate for the procedure.

Abdominoplasty, commonly known as a tummy tuck, is a surgical procedure designed to remove excess fat and skin from the abdominal area and tighten the abdominal muscles. This procedure is often performed for individuals who have experienced significant weight loss, pregnancy, or aging, and it aims to restore a smoother, firmer abdominal profile.
During an abdominoplasty, the surgeon makes an incision along the lower abdomen, often just above the pubic area. The excess skin and fat are removed, and the abdominal muscles, which may have been stretched or weakened, are tightened. In some cases, liposuction may also be used to remove additional fat in the area.
.Full Abdominoplasty : Involves a larger incision to remove more skin and fat and is often combined with muscle tightening for comprehensive contouring.
.Mini Abdominoplasty : A smaller incision for individuals who only have excess skin below the belly button. This procedure typically does not involve muscle tightening.
.Extended Abdominoplasty : Often done for patients who have undergone significant weight loss. The incision may extend around the back to remove excess skin from the flanks as well.
.Improves the contour and appearance of the abdomen.
.Removes excess skin and fat after pregnancy or weight loss.
.Strengthens the abdominal muscles, restoring tone and firmness.
.Can help improve posture and relieve back pain caused by weak abdominal muscles.
As with any major surgery, there are risks, including:
.Infection
.Scarring
.Blood clots
.Excessive bleeding or fluid buildup
.Changes in skin sensation
.Uneven results or asymmetry
After the procedure, patients will need to wear compression garments to help reduce swelling and support the healing process. There will be discomfort and swelling, but this can be managed with pain medications. It’s crucial to avoid strenuous activity for several weeks. Most people can return to work after 2-4 weeks, but full recovery may take up to 6 months.
Ideal candidates for abdominoplasty include individuals who:
.Are in good overall health
.Have excess skin and fat in the abdominal area
.Have had significant weight loss or pregnancy and want to restore their body shape
.ave realistic expectations about the results
If you’re considering abdominoplasty, it’s essential to consult with a board-certified plastic surgeon. They will evaluate your health, discuss your goals, and help determine if this procedure is right for you.
Fat Grafting, also known as fat transfer, is a cosmetic procedure where fat is taken from one part of the body (often areas with excess fat, like the abdomen or thighs) and injected into another part of the body to restore volume, smooth wrinkles, or enhance contour. It's a natural, long-lasting way to enhance various body areas using the patient's own fat tissue.
The procedure involves the following steps:
.Fat Harvesting : Fat is collected from a donor area (such as the abdomen, thighs, or flanks) using liposuction.
.Purification : The harvested fat is purified to remove any impurities, excess fluid, or blood.
.Fat Injection : The purified fat is injected into the target area, such as the face, breasts, or buttocks, to enhance volume and contour.
.Healing : The transferred fat cells integrate into the surrounding tissue, providing a natural, lasting result.
.Facial Rejuvenation : Fat grafting is commonly used to restore volume to the face, reducing wrinkles and hollow areas (such as under the eyes or in the cheeks).
.Breast Augmentation : Fat transfer can be used for natural breast enlargement or correction of post-surgical breast irregularities.
.Body Contouring : Fat is injected into areas like the buttocks (Brazilian Butt Lift) or hips to improve contour and shape.
.Scar Correction : It can also be used to improve the appearance of scars or skin depressions caused by trauma or burns.
.Natural and long-lasting results using the patient’s own tissue.
.Helps enhance body contours or facial features without the need for synthetic implants.
.Dual benefit: Liposuction removes fat from unwanted areas while enhancing other areas with the same fat.
.Low risk of allergic reactions as the procedure uses the patient’s own fat.
Although fat grafting is generally safe, as with any surgery, there are some risks, including:
.Infection
.Bruising and swelling at both the donor and recipient sites
.Fat absorption: Some of the transferred fat may be reabsorbed by the body.
.Asymmetry or uneven results in the recipient area
.Lumps or irregularities if fat is not distributed evenly
Recovery varies depending on the areas treated. Here’s what to expect:
.Compression garments are typically worn to minimize swelling in the donor area and support the healing process.
.Swelling and bruising are common and can take several weeks to subside.
.Patients may need to avoid strenuous physical activity for several weeks during recovery.
.Most people return to work within a few days to a week, but full recovery can take several months.
Ideal candidates for fat grafting include:
.Individuals with excess fat in areas like the abdomen or thighs, which can be used for transfer.
.Patients seeking a natural, non-surgical alternative to implants or fillers.
.People who have realistic expectations about the results and the potential need for touch-ups.
.Those in good overall health with no contraindications for surgery.
If you’re interested in fat grafting, it’s important to consult with a board-certified plastic surgeon. They will assess your suitability for the procedure, discuss your aesthetic goals, and help you understand what you can expect from the results.
Breast implants are medical devices used in cosmetic surgery to enhance the size, shape, or fullness of a woman’s breasts. They are typically used for breast augmentation or reconstruction after mastectomy (breast cancer surgery). The procedure involves placing implants filled with either saline or silicone gel under the breast tissue or chest muscles.
.Saline Implants: These are filled with sterile salt water (saline). They are inserted empty and then filled after placement. They can be adjusted for size during the procedure.
.Silicone Gel Implants: These are pre-filled with a thick silicone gel that closely mimics the feel of natural breast tissue. They are often preferred for a more natural feel.
.Gummy Bear Implants: These are a type of silicone implant with a cohesive gel that holds its shape, reducing the risk of leakage or rupture.
.Structured Implants: These are filled with saline but have an inner structure that mimics the natural feel of breast tissue more than regular saline implants.
During breast implant surgery, a surgeon will make an incision in one of the following areas:
.Inframammary Fold (under the breast): The most common incision site, which results in minimal visible scarring.
.Periareolar (around the nipple): The incision is made around the edge of the areola. This technique may leave less visible scars, especially for women with darker areolas.
.Transaxillary (through the armpit): This incision is made in the armpit, leaving no scars on the breast. However, this method may be less precise and can involve longer recovery.
.Enhances breast size, shape, and volume for a fuller appearance.
.Helps restore breast volume and symmetry after weight loss, pregnancy, or mastectomy.
.Can boost self-esteem and confidence in women who are dissatisfied with their breast size.
.Offers a variety of sizes and shapes to achieve a natural or more augmented look depending on personal preference.
As with any surgical procedure, breast implant surgery carries certain risks and potential complications, including:
.Infection
.Capsular contracture (scar tissue around the implant causing firmness and distortion)
.Implant rupture or leakage
.Changes in breast sensation (nipple or breast tissue)
.Breast asymmetry
.Wrinkling or rippling of the implant, especially in saline implants
.Possible need for revision surgery or implant replacement after a few years
Recovery time can vary, but in general, patients can expect:
.Wearing a supportive bra or compression garment to reduce swelling and support healing.
.Swelling, bruising, and discomfort in the first few days after surgery.
.Resuming light activities after 1-2 weeks, with full recovery taking up to 6 weeks or longer, depending on individual healing rates.
.Avoiding heavy lifting and strenuous activities for several weeks post-surgery to ensure proper healing.
Ideal candidates for breast implants include women who:
.Are in good overall health and have realistic expectations.
.Desire breast enhancement for cosmetic reasons or to restore breast volume after pregnancy, weight loss, or surgery.
.Are not pregnant or breastfeeding.
.Have adequate skin elasticity to support implants.
If you're considering breast implants, it's important to consult with a board-certified plastic surgeon who specializes in breast surgery. They will evaluate your health, understand your aesthetic goals, and help you choose the best implant type, size, and placement for your body.
Breast reconstruction is a surgical procedure designed to restore the shape, appearance, and size of the breast after a mastectomy (breast removal surgery), typically due to breast cancer. The goal is to help individuals regain a natural-looking breast and improve self-esteem and body image following the loss of a breast.
.Implant-Based Reconstruction: Involves the use of breast implants to rebuild the breast mound. The procedure can be done immediately after mastectomy or later, and the implants can be filled with saline or silicone gel.
.Autologous (Flap) Reconstruction: Uses tissue from another part of your body (such as the abdomen, back, or thighs) to reconstruct the breast. This method provides a more natural feel as it uses your own tissue.
.Combination of Implant and Flap Reconstruction: Sometimes, a combination of flap surgery and breast implants is used to achieve a more natural breast shape and volume.
.Oncoplastic Reconstruction: This technique combines breast cancer surgery with breast reduction or lift, often used to balance the appearance of the remaining breast tissue after the mastectomy.
The specific method used depends on several factors, including the patient’s health, breast cancer treatment, and personal preferences. During the procedure:
.For implant-based reconstruction, the surgeon will create a pocket in the chest to place the implant, either right away (immediate reconstruction) or later (delayed reconstruction).
.For flap-based reconstruction, tissue is taken from another area of your body, such as the abdomen (DIEP flap) or back (LAT flap), to create a new breast mound.
.In some cases, nipple and areola reconstruction can be done later to complete the breast’s appearance.
.Restores a natural-looking breast after mastectomy.
.Can improve self-esteem and body image by recreating the appearance of a full breast.
.Provides an option for women who want to avoid the need for external prostheses (breast forms).
.Reconstruction can be performed immediately after mastectomy or later, depending on the individual's health and cancer treatment.
Like any surgery, breast reconstruction has its risks. These may include:
.Infection at the surgical site
.Bleeding or fluid accumulation (seroma)
.Scarring
.Flap failure (in flap reconstruction, where the transferred tissue doesn't survive or heal well)
.Implant complications, such as rupture, shifting, or capsular contracture (tightening of scar tissue around the implant)
.Nipple and areola reconstruction may not look identical to the original breast tissue
.Longer recovery times, especially for flap surgeries
The recovery process varies depending on the type of surgery, but in general:
.You will likely experience swelling, bruising, and discomfort after the surgery, which can be managed with pain medications.
.For implant-based reconstruction, you may need to wear a supportive bra or compression garment for several weeks.
.Flap-based reconstruction typically requires a longer recovery time, as tissue from other parts of the body is used. Full recovery can take several months.
.Physical therapy may be needed for patients who had tissue taken from their abdomen, back, or thighs to help regain strength and mobility in those areas.
.It may take a few months to return to full physical activities, but most patients can resume normal activities after 6-8 weeks.
Ideal candidates for breast reconstruction include women who:
.Have undergone a mastectomy (breast removal surgery) due to breast cancer or other medical conditions.
.Are in good overall health and have a stable medical condition.
.Have realistic expectations about the outcome of the surgery.
.Are committed to following the post-surgery recovery plan and attend follow-up appointments.
If you are considering breast reconstruction, it’s essential to consult with a board-certified plastic surgeon who specializes in breast surgery. The surgeon will evaluate your individual needs, explain the available options, and develop a personalized treatment plan based on your health, preferences, and the results of your cancer treatment.
Breast reduction surgery, also known as reduction mammoplasty, is a procedure aimed at reducing the size and volume of overly large breasts. The surgery removes excess breast tissue, fat, and skin to create a smaller, more proportional breast size. This procedure is often performed to alleviate physical discomfort, improve body proportions, and enhance self-confidence.
.Physical Discomfort: Large breasts can cause chronic neck, back, and shoulder pain, poor posture, and skin irritation.
.Difficulty in Physical Activities: Large breasts can limit a person's ability to participate in physical activities and exercise comfortably.
.Emotional or Psychological Reasons: Some women may feel self-conscious about the size of their breasts and desire a more proportionate appearance to improve body image and self-esteem.
During breast reduction surgery, the surgeon makes incisions around the areola, vertically down the breast, and along the breast crease. Through these incisions:
.The surgeon removes excess tissue, fat, and skin.
.The remaining tissue is reshaped to create a smaller, more youthful breast shape.
.The nipple and areola are repositioned to a higher, more natural position.
.If necessary, liposuction may be used to remove fat from the surrounding areas for more even results.
.Traditional Breast Reduction: The most common technique, involving an anchor-shaped incision around the areola, down the center, and under the breast.
.Liposuction Breast Reduction: A less invasive option for individuals with more fatty tissue than glandular tissue, where excess fat is removed through small incisions using a suction device.
.Vertical Breast Reduction (Short Scar): Involves fewer incisions, typically around the areola and down the center of the breast, making it a less invasive option for some patients.
.Relieves physical discomfort such as neck, back, and shoulder pain.
.Improves posture by alleviating the strain caused by heavy breasts.
.Enhances body proportions and symmetry, helping the individual achieve a more balanced appearance.
.Improves self-confidence and body image for women who feel self-conscious about their large breasts.
.May make it easier to engage in physical activities and exercise comfortably.
As with any surgery, breast reduction has potential risks and complications. These may include:
.Infection
.Bleeding
.Changes in nipple or breast sensation
.Scarring
.Uneven or asymmetrical results
.Problems with breastfeeding, as the surgery may affect milk ducts
.Slow healing or delayed wound closure
After breast reduction surgery, patients will need to follow specific recovery instructions to ensure proper healing:
.You may experience swelling, bruising, and discomfort, which can be managed with pain medications.
.A surgical bra or compression garment will be worn to support the breasts during the healing process.
.It’s important to avoid strenuous activities, heavy lifting, and physical exercise for several weeks.
.Most people can return to work and normal activities after 2-4 weeks, although full recovery may take up to 6 months.
.Follow-up appointments will be necessary to monitor healing and ensure there are no complications.
Ideal candidates for breast reduction are women who:
.Have large breasts causing physical discomfort, such as back, neck, and shoulder pain.
.Have realistic expectations about the outcome of the surgery.
.Are in good overall health and do not have any conditions that could interfere with the healing process.
.Are bothered by the size or appearance of their breasts and wish to achieve a more proportionate figure.
.Are finished with breastfeeding, as the surgery can impact milk production.
If you're considering breast reduction, it’s important to consult with a board-certified plastic surgeon who specializes in breast surgery. They will assess your physical health, discuss your goals, and help determine if breast reduction surgery is right for you.

A split ear lobule is a condition where the soft, fleshy part of the ear (the earlobe) becomes torn or split. This can happen due to various reasons, including trauma, wearing heavy earrings, or prolonged use of large jewelry. Split ear lobules can be distressing, both aesthetically and physically, but they can be repaired with a relatively simple surgical procedure.
.Trauma: Accidental injury, such as pulling on earrings or earrings getting caught in clothing or hair, can cause the ear lobe to tear.
.Heavy Earrings: Prolonged use of heavy earrings or jewelry, especially those that stretch the earlobe, can lead to splitting.
.Large Gauge Piercings: Stretching the ear lobes through large gauge piercings can sometimes result in the ear lobe splitting over time.
.Infections: Infections from piercings can cause the tissue to weaken and tear.
.Visible tear or split in the earlobe.
.Swelling, redness, or pain around the torn area (especially if caused by trauma or infection).
.In some cases, the earlobe may become enlarged or elongated due to stretching or repeated injury.
Treatment for a split ear lobule typically depends on the severity of the tear:
.Conservative Treatment : If the split is small and the ear is otherwise healthy, the tear may heal naturally with proper care and avoiding further trauma.
.Surgical Repair : For more severe splits or tears, a minor surgical procedure can be performed to stitch the ear back together. This procedure is usually done under local anesthesia and takes about 30 minutes to complete.
.Ear Lobe Reconstruction : In cases where the earlobe is significantly damaged or stretched, further reconstructive surgery may be needed to restore the shape and appearance of the earlobe.
.Restores the appearance of the earlobe, making it look symmetrical and natural.
.Reduces physical discomfort caused by the split or tear.
.Prevents further tearing or damage to the ear lobe tissue.
.Allows for the safe use of earrings or jewelry without the risk of exacerbating the tear.
Like any surgical procedure, repairing a split ear lobule carries some risks and complications, including:
.Infection
.Scarring or uneven healing
.Recurrence of the tear if the ear is subjected to further trauma
.Changes in the shape or size of the earlobe post-surgery
Recovery from split ear lobule surgery is generally quick and straightforward. After the procedure:
.You may experience some mild swelling, bruising, or discomfort, which can be managed with over-the-counter pain relievers.
.It’s important to avoid putting pressure on the ear or wearing earrings until the area has fully healed (usually 2-4 weeks).
.Follow-up appointments with the surgeon may be needed to monitor the healing process and ensure there are no complications.
Ideal candidates for split ear lobule repair are individuals who:
.Have experienced a tear or split in the earlobe due to trauma or other causes.
.Want to restore the appearance of the earlobe for aesthetic or functional reasons (e.g., to wear earrings again).
.Are in good overall health and have realistic expectations about the outcome of the surgery.
If you experience a split ear lobule, it’s important to consult a medical professional, such as a plastic surgeon, for proper diagnosis and treatment. Timely intervention can prevent further damage and help you restore the appearance of your ear lobe.

Post wound healing treatment is a crucial phase in the recovery process following an injury, surgery, or any kind of skin trauma. Effective care during this phase ensures optimal recovery, reduces complications like infections or scarring, and promotes healthy tissue regeneration. Various factors such as nutrition, wound care, and lifestyle can impact the healing process.
Wound healing typically progresses in four overlapping phases:
.Hemostasis (Blood Clotting) : Immediately after the injury, the body works to stop the bleeding by forming a clot.
.Inflammatory Phase : In this phase, white blood cells work to prevent infection by clearing out dead tissue and bacteria.
.Proliferative Phase : This phase focuses on tissue growth. New blood vessels form, and the wound starts to fill with new tissue.
.Remodeling Phase : The final phase, where collagen is reorganized, and the wound strengthens, becoming more resilient and less noticeable.
Proper treatment can help promote faster healing and prevent complications. Here are common treatments for post-wound healing:
.Wound Care : Regular cleaning and dressing of the wound are essential to prevent infection. Depending on the severity, dressing changes may be done daily or as prescribed by the healthcare provider.
.Antibiotics : If there is a risk of infection, antibiotics may be prescribed to prevent bacterial infections. Topical or oral antibiotics may be used depending on the condition.
.Moist Wound Healing : Keeping the wound moist (rather than allowing it to dry out) promotes faster and more effective healing by maintaining a moist environment that encourages tissue growth.
.Pressure Relief (for Bedsores or Ulcers): Using pressure-relieving devices like specialized mattresses, cushions, or dressings can prevent further injury and reduce pressure on the wound, especially for individuals with immobility issues.
.Hydrotherapy : Hydrotherapy treatments, such as using water or saline to irrigate and cleanse the wound, can help remove dead tissue and promote healthy tissue regeneration.
.Skin Grafting : In severe cases of skin damage, a skin graft may be performed. This involves taking healthy skin from another part of the body and transplanting it to the wound site to aid healing.
Nutrition plays a vital role in wound healing. Essential nutrients that support recovery include:
.Proteins : Vital for tissue repair and immune function. Good sources include lean meats, fish, eggs, and legumes.
.Vitamin C : Crucial for collagen formation and tissue repair. Found in citrus fruits, strawberries, and leafy greens.
.Zinc : Plays a role in cell growth and immune function. Rich sources include nuts, seeds, and whole grains.
.Vitamin A : Supports immune function and tissue repair. Found in carrots, sweet potatoes, and leafy vegetables.
.Hydration : Proper hydration helps maintain skin elasticity and supports the overall healing process.
.Age : Older adults often have slower wound healing due to a decline in cellular regeneration.
.Chronic Conditions : Conditions like diabetes, vascular diseases, or immunodeficiency can impair the body’s ability to heal wounds efficiently.
.Smoking : Smoking decreases blood flow and oxygenation, which can significantly slow the healing process.
.Nutrition : A poor diet can delay healing, while good nutrition supports faster and more effective recovery.
.Infection : The presence of infection can delay healing and may require medical intervention.
Several complications may arise during post-wound healing, including:
.Infection : If a wound is not properly cared for, it can become infected, which can delay healing and lead to more severe health issues.
.Delayed Healing : Certain conditions, such as poor circulation, can cause wounds to heal slowly or fail to heal altogether.
.Scarring : While some scarring is natural, excessive scarring (keloids or hypertrophic scars) may occur, especially if the wound is not cared for properly.
.Chronic Wounds : Some wounds, especially pressure ulcers or diabetic foot ulcers, can become chronic and require specialized care to heal completely.
It's important to seek medical help if you notice any of the following during post-wound healing:
.Increased redness, swelling, or warmth around the wound
.Discharge of pus or other fluids from the wound
.Fever or chills (signs of infection)
.Wound edges that do not close or heal properly
.Severe pain or a worsening condition

Post wound healing treatment is a crucial phase in the recovery process following an injury, surgery, or any kind of skin trauma. Effective care during this phase ensures optimal recovery, reduces complications like infections or scarring, and promotes healthy tissue regeneration. Various factors such as nutrition, wound care, and lifestyle can impact the healing process.
Wound healing typically progresses in four overlapping phases:
.Hemostasis (Blood Clotting) : Immediately after the injury, the body works to stop the bleeding by forming a clot.
.Inflammatory Phase : In this phase, white blood cells work to prevent infection by clearing out dead tissue and bacteria.
.Proliferative Phase : This phase focuses on tissue growth. New blood vessels form, and the wound starts to fill with new tissue.
.Remodeling Phase : The final phase, where collagen is reorganized, and the wound strengthens, becoming more resilient and less noticeable.
Proper treatment can help promote faster healing and prevent complications. Here are common treatments for post-wound healing:
.Wound Care : Regular cleaning and dressing of the wound are essential to prevent infection. Depending on the severity, dressing changes may be done daily or as prescribed by the healthcare provider.
.Antibiotics : If there is a risk of infection, antibiotics may be prescribed to prevent bacterial infections. Topical or oral antibiotics may be used depending on the condition.
.Moist Wound Healing : Keeping the wound moist (rather than allowing it to dry out) promotes faster and more effective healing by maintaining a moist environment that encourages tissue growth.
.Pressure Relief (for Bedsores or Ulcers): Using pressure-relieving devices like specialized mattresses, cushions, or dressings can prevent further injury and reduce pressure on the wound, especially for individuals with immobility issues.
.Hydrotherapy : Hydrotherapy treatments, such as using water or saline to irrigate and cleanse the wound, can help remove dead tissue and promote healthy tissue regeneration.
.Skin Grafting : In severe cases of skin damage, a skin graft may be performed. This involves taking healthy skin from another part of the body and transplanting it to the wound site to aid healing.
Nutrition plays a vital role in wound healing. Essential nutrients that support recovery include:
.Proteins : Vital for tissue repair and immune function. Good sources include lean meats, fish, eggs, and legumes.
.Vitamin C : Crucial for collagen formation and tissue repair. Found in citrus fruits, strawberries, and leafy greens.
.Zinc : Plays a role in cell growth and immune function. Rich sources include nuts, seeds, and whole grains.
.Vitamin A : Supports immune function and tissue repair. Found in carrots, sweet potatoes, and leafy vegetables.
.Hydration : Proper hydration helps maintain skin elasticity and supports the overall healing process.
.Age : Older adults often have slower wound healing due to a decline in cellular regeneration.
.Chronic Conditions : Conditions like diabetes, vascular diseases, or immunodeficiency can impair the body’s ability to heal wounds efficiently.
.Smoking : Smoking decreases blood flow and oxygenation, which can significantly slow the healing process.
.Nutrition : A poor diet can delay healing, while good nutrition supports faster and more effective recovery.
.Infection : The presence of infection can delay healing and may require medical intervention.
Several complications may arise during post-wound healing, including:
.Infection : If a wound is not properly cared for, it can become infected, which can delay healing and lead to more severe health issues.
.Delayed Healing : Certain conditions, such as poor circulation, can cause wounds to heal slowly or fail to heal altogether.
.Scarring : While some scarring is natural, excessive scarring (keloids or hypertrophic scars) may occur, especially if the wound is not cared for properly.
.Chronic Wounds : Some wounds, especially pressure ulcers or diabetic foot ulcers, can become chronic and require specialized care to heal completely.
It's important to seek medical help if you notice any of the following during post-wound healing:
.Increased redness, swelling, or warmth around the wound
.Discharge of pus or other fluids from the wound
.Fever or chills (signs of infection)
.Wound edges that do not close or heal properly
.Severe pain or a worsening condition
A pre-pregnancy checkup is essential for both partners to ensure a healthy start to conception. It involves a comprehensive review of your health, lifestyle, and fertility to address potential risks and increase the chances of a smooth pregnancy.
Pre-pregnancy checkups are important for :
.Health Optimization : Preparing your body for conception by addressing any underlying health issues like diabetes, hypertension, or hormonal imbalances.
.Fertility Readiness : Identifying and treating issues related to fertility for both men and women to increase the chances of successful conception.
.Risk Prevention : Identifying any health concerns or infections that could affect pregnancy or fetal development, such as Rubella, Hepatitis, or sexually transmitted diseases.
.Medical History Review: Discuss any chronic conditions (e.g., diabetes, hypertension) and past pregnancies or reproductive health issues.
.Physical Examination: Includes weight and BMI check, blood pressure monitoring, and pelvic exam for women.
.Blood Tests & Screenings: To check blood type, hemoglobin, infectious diseases (e.g., HIV, Hepatitis), and genetic disorders.
.Fertility Assessment: Reviewing ovulation, sperm count (for men), and other fertility-related factors.
.Folic Acid: Vital for neural tube development. Start taking 400-800 mcg per day before pregnancy.
.Iron & Calcium: Iron helps prevent anemia, and calcium supports bone health.
.Vitamin D: Ensures proper bone and immune function.
.Preconception Counseling: For genetic conditions or family history concerns.
.Maintain a Healthy Weight: Optimal weight is crucial for fertility and pregnancy health.
.Quit Smoking and Avoid Alcohol: Both habits affect fertility and pregnancy outcomes.
.Exercise Regularly: Regular physical activity helps improve overall health and fertility.
It is recommended to schedule a pre-pregnancy checkup **3-6 months before trying to conceive**. This gives enough time to address any medical concerns, improve fertility, and optimize health.
Normal delivery, also known as vaginal birth, is a natural process where the baby is born through the birth canal (vagina). This is the most common and natural form of childbirth. It typically requires no surgical intervention unless complications arise.
Normal delivery occurs in three main stages :
.First Stage (Labor): This is the longest stage, during which the cervix dilates (opens) to 10 cm. It can last anywhere from several hours to a full day. This stage has three phases:
.Second Stage (Pushing and Delivery): The baby moves down the birth canal and is born. The mother will push during contractions, and the healthcare provider will assist in guiding the baby out.
.Third Stage (After Birth): This stage involves the delivery of the placenta. Contractions continue to help expel the placenta after the baby is born.
Normal delivery has several benefits for both the mother and the baby:
.Shorter Recovery Time: Compared to cesarean delivery, mothers who have a normal delivery often recover faster and can get back to daily activities sooner.
.Lower Risk of Infection: Vaginal delivery involves no incisions, reducing the risk of infection compared to C-sections.
.Stronger Bonding with Baby: The physical contact during vaginal birth, including skin-to-skin contact immediately after birth, helps establish early bonding and breastfeeding.
.Health Benefits for Baby: Passing through the birth canal helps clear the baby’s airways and improves lung function.
While normal delivery is generally safe, there are some risks involved:
.Perineal Tears : The area between the vagina and anus (perineum) may tear during childbirth. Most tears are minor, but some may require stitches.
.Postpartum Hemorrhage : Excessive bleeding after birth can occur, but it can usually be managed with medical intervention.
.Shoulder Dystocia : This occurs when the baby’s shoulder gets stuck during delivery. While rare, it requires prompt medical attention to prevent injury.
.Fetal Distress : Occasionally, the baby may experience a lack of oxygen during labor, necessitating a change in delivery plan or interventions such as assisted delivery or C-section.

A Caesarean Section (C-Section) is a surgical procedure in which a baby is delivered through an incision made in the mother's abdomen and uterus, rather than through the birth canal (vagina). It is typically performed when a vaginal delivery would pose a risk to the health of the mother or baby.
A C-section may be recommended in the following situations :
.Labor Is Not Progressing: If the cervix isn't opening (dilating) enough or the baby isn’t descending in the birth canal, a C-section may be needed.
.Fetal Distress: If the baby is not getting enough oxygen or shows signs of distress during labor, a C-section may be necessary.
.Multiple Births: In the case of twins or higher-order multiples, a C-section may be recommended for safe delivery.
.Placenta Complications: If the placenta is blocking the cervix (placenta previa) or if it detaches prematurely (placental abruption), a C-section might be necessary.
.Previous C-Section: Women who have had a C-section in the past may require another C-section for subsequent deliveries to avoid the risk of uterine rupture.
A C-section typically follows these steps:
.Anesthesia : An epidural or spinal block is administered to numb the lower half of the body, so the mother remains awake during the procedure.
.Incision : The surgeon makes a horizontal incision in the lower abdomen and another in the uterus to access the baby.
.Delivery : The baby is gently lifted out of the uterus and handed over to the pediatric team for evaluation.
.Closing the Incision : Once the baby is delivered, the uterus and abdomen are stitched up, and the mother is moved to the recovery room.
Some of the key benefits of a C-section include:
.Planned Procedure : A C-section can be scheduled in advance, which may help reduce stress and anxiety about labor and delivery.
.Less Risk of Birth Injury : It reduces the risk of injuries like shoulder dystocia or umbilical cord prolapse during vaginal birth.
.Quick Access to Medical Intervention : A C-section is useful in emergency situations where immediate intervention is required to save the life of the mother or baby.
While a C-section is often necessary to ensure the safety of the mother and baby, it should be considered carefully with a healthcare provider. If you have concerns or would like to learn more about your delivery options, consult your obstetrician or healthcare team.

**Painless Normal Delivery**, also known as **Epidural Analgesia**, is a method used to provide pain relief during labor and childbirth. It allows the mother to experience vaginal birth without the intense pain typically associated with contractions and delivery.
The most common technique for painless delivery is **epidural anesthesia**, where a local anesthetic is injected into the epidural space of the spine. This blocks the pain from contractions while allowing the mother to remain awake and alert.
.Effective Pain Relief: Helps manage pain during labor without the need for oral medication.
.Alertness and Participation: The mother stays awake and can actively participate in the birth.
.Reduces Stress and Anxiety: Helps women feel more relaxed and less anxious about the labor process.
Painless normal delivery can be used in most cases of vaginal childbirth, especially when:
.Labor Is Well-Progressed: Usually after the cervix is dilated 3-4 cm.
.No Health Contraindications: Women with conditions such as spinal issues, allergies to anesthesia, or infections may not be eligible for an epidural.
While painless delivery is generally safe, some risks and side effects may include:
.Lower Blood Pressure: Epidurals may cause a drop in blood pressure, affecting both the mother and baby.
.Back Pain: Some women report soreness or back pain after the epidural.
.Difficulty Pushing: The mother might find it harder to feel contractions or push effectively due to the numbing effects.
Painless normal delivery offers a more comfortable birth experience by minimizing labor pain. However, it is important to discuss with your healthcare provider whether this method is suitable for you, considering your medical history and pregnancy condition.
Laparoscopic Tubectomy, also known as tubal ligation, is a surgical procedure in which a woman’s fallopian tubes are blocked, cut, or sealed to prevent pregnancy. This is considered a permanent method of contraception. The procedure is performed using a laparoscope, a small, thin tube with a camera, which allows the surgeon to make small incisions and work with minimal invasiveness.
Laparoscopic Tubectomy is typically chosen for the following reasons:
.Permanent Contraception : Women who have completed their family and wish to avoid future pregnancies.
.Health Conditions : For women with health conditions that would make pregnancy dangerous.
.Birth Control Failure : For women who have experienced failure with other forms of contraception.
Some of the key benefits of laparoscopic tubectomy include:
.Effective Permanent Birth Control : Provides a highly effective, permanent solution for preventing pregnancy.
.Minimally Invasive : The laparoscopic technique involves small incisions, resulting in less pain and faster recovery compared to traditional surgery.
.Short Recovery Time: The procedure typically allows for a quicker recovery and return to daily activities.
The procedure is typically done under general anesthesia or regional anesthesia. Here are the general steps of the laparoscopic tubectomy:
.Incision and Insertion of Laparoscope: The surgeon makes a small incision near the belly button and inserts the laparoscope to view the fallopian tubes.
.Fallopian Tube Treatment: Depending on the method chosen, the fallopian tubes may be cut, tied, or sealed using clips or cauterization.
.Closing Incisions: After the procedure is completed, the incisions are closed, and the patient is moved to a recovery room.
Laparoscopic Tubectomy is a safe and effective permanent contraception option for women who are certain they do not want more children. It is minimally invasive and allows for a quick recovery. However, as it is permanent, it is crucial to carefully consider all aspects of this decision and consult with a healthcare professional.
Laparoscopic Hysterectomy is a minimally invasive surgery in which the uterus is removed through small incisions made in the abdomen using a laparoscope (a small tube with a camera). This procedure is often recommended for women who have conditions such as fibroids, abnormal bleeding, or cancer.
Laparoscopic hysterectomy may be recommended in the following situations:
.Uterine Fibroids : Benign growths in the uterus causing pain or bleeding.
.Endometriosis : A condition where tissue similar to the uterine lining grows outside the uterus.
.Abnormal Bleeding : Chronic heavy or irregular bleeding that doesn't respond to other treatments.
.Cancer : Uterine or cervical cancer when the uterus needs to be removed.
Some of the benefits of laparoscopic hysterectomy include:
.Minimally Invasive: Smaller incisions lead to less pain and a faster recovery compared to traditional open surgery.
.Shorter Recovery Time: Typically, recovery time is quicker, allowing women to return to daily activities sooner.
.Less Scarring: The small incisions result in minimal scarring.
The procedure generally involves the following steps:
.Anesthesia: General anesthesia is administered so the patient is asleep and pain-free during the procedure.
.Incisions: Several small incisions are made in the abdomen, through which the laparoscope and surgical instruments are inserted.
.Removal of the Uterus: The uterus is carefully separated from surrounding tissues and removed through one of the incisions.
.Closing the Incisions: After removal, the incisions are closed using stitches or staples.
Laparoscopic hysterectomy is an effective option for treating various uterine conditions. It offers significant advantages over traditional open surgery, including shorter recovery time, minimal scarring, and reduced hospital stays. However, like any surgical procedure, it is essential to consider the potential risks and consult with a healthcare provider for personalized advice.
Diagnostic Laparoscopy and Hysteroscopy (Lap-Hysteroscopy) is a minimally invasive procedure that combines two diagnostic techniques: laparoscopy and hysteroscopy. The procedure allows doctors to examine the internal organs of the female reproductive system (the uterus, ovaries, fallopian tubes, and surrounding pelvic organs) for potential issues such as fibroids, endometriosis, scarring, and other abnormalities.
- laparoscopy involves inserting a small camera (laparoscope) through a small incision in the abdomen to view the abdominal and pelvic organs. - Hysteroscopy involves inserting a thin, lighted tube (hysteroscope) into the uterus through the cervix to examine the uterine lining and internal structures.
Diagnostic lap-hysteroscopy is often recommended for women who are experiencing unexplained infertility or recurrent miscarriages, or who have abnormal findings from other diagnostic tests. It is also used to:
.Assess Pelvic Pain: To investigate causes of pelvic pain, such as endometriosis, pelvic adhesions, or fibroids.
.Investigate Infertility: To examine potential causes of infertility like blocked fallopian tubes, fibroids, or endometrial polyps.
Some of the benefits of diagnostic lap-hysteroscopy include:
.Minimally Invasive: Both procedures are minimally invasive, involving small incisions, which leads to less discomfort and faster recovery.
.Diagnostic Accuracy: Provides a comprehensive view of both the pelvic cavity and the uterine cavity for accurate diagnosis.
.Treatment Option: In some cases, therapeutic procedures like removing fibroids, polyps, or adhesions can be performed during the same procedure.
Although lap-hysteroscopy is a safe procedure, it carries some risks, such as:
.Infection : Risk of infection in the uterus, abdomen, or pelvic region.
.Bleeding : Some bleeding during or after the procedure is common, though significant bleeding is rare.
.Injury to Organs : There is a slight risk of injury to surrounding organs, such as the bladder, bowel, or blood vessels.
.Gas Embolism : Rarely, the gas used to inflate the abdomen can enter the bloodstream, leading to a serious condition called gas embolism.
Diagnostic lap-hysteroscopy is a highly effective and minimally invasive procedure that offers a detailed view of the reproductive organs. It allows doctors to identify and treat a wide range of conditions affecting the pelvic region and uterus. It is a valuable tool in evaluating infertility, abnormal bleeding, pelvic pain, and other gynecological issues. If you have been advised to undergo this procedure, it’s important to discuss your medical history and any concerns with your healthcare provider.
Vaginal Hysterectomy is a surgical procedure in which the uterus is removed through the vagina. This method is generally preferred over abdominal hysterectomy due to its shorter recovery time, reduced risk of infection, and smaller scars. It is often performed for conditions such as uterine fibroids, cancer, or severe uterine prolapse.
Vaginal hysterectomy may be recommended for various reasons, including:
.Uterine Fibroids: Non-cancerous growths in the uterus that cause pain, bleeding, or pressure on surrounding organs.
.Uterine Prolapse: When the uterus drops into the vaginal canal due to weakened pelvic muscles and ligaments.
.Endometriosis: A condition where tissue similar to the lining inside the uterus grows outside of it, causing pain and infertility.
.Cancer: Uterine cancer, cervical cancer, or ovarian cancer that requires removal of the uterus.
The procedure involves the following steps:
.Anesthesia: The patient is given general anesthesia or regional anesthesia to ensure they are comfortable and pain-free during the surgery.
.Incision: A small incision is made inside the vaginal canal. The uterus is then carefully separated from surrounding structures such as the cervix, ovaries, and ligaments.
.Removal of Uterus: The uterus is removed through the vaginal opening. In some cases, the cervix may also be removed.
Vaginal hysterectomy is a highly effective procedure with a low risk of complications when performed by an experienced surgeon. It offers many advantages over abdominal hysterectomy, particularly in terms of recovery time and cosmetic outcome.
Infertility treatment refers to medical procedures and interventions aimed at helping individuals or couples conceive when they are unable to do so naturally. There are various causes of infertility, and treatments can vary depending on the underlying issues. Common treatments include medication, surgery, assisted reproductive technologies (ART), and lifestyle changes.
Infertility treatment may be recommended for couples who have been unable to conceive after 12 months of regular, unprotected intercourse (or 6 months for women over 35). Common causes for infertility include:
.Ovulatory Disorders: Irregular ovulation or anovulation (lack of ovulation) can prevent pregnancy.
.Fallopian Tube Blockage: Blocked or damaged fallopian tubes can prevent the sperm from reaching the egg.
Infertility treatments can be broadly categorized into medical treatments and assisted reproductive technologies (ART):
.Medication: Hormonal treatments like Clomid or gonadotropins are commonly used to regulate ovulation.
.Intrauterine Insemination (IUI): Sperm is directly injected into the uterus around the time of ovulation to improve the chances of fertilization.
.In Vitro Fertilization (IVF): Eggs are retrieved, fertilized in a lab, and then implanted in the uterus.
The main benefit of infertility treatment is the possibility of achieving a successful pregnancy. Additional benefits include:
.Improved Chances of Pregnancy: Treatments like IVF or IUI increase the likelihood of conception for couples facing infertility.
.Personalized Approach: Fertility treatments are tailored based on individual diagnoses and conditions.
Infertility treatment offers hope to many couples and individuals struggling with conception. Though it can be a complex and sometimes lengthy process, modern fertility treatments have helped millions of people achieve their dreams of parenthood.
Uterine cancer is a type of cancer that begins in the lining of the uterus, known as the endometrium. It is one of the most common types of cancer affecting the female reproductive system. Early detection and prompt treatment are key to improving the chances of successful outcomes.
Uterine cancer is often suspected when a woman experiences unusual symptoms. These can include:
.Abnormal Vaginal Bleeding: This can be in the form of heavy or irregular periods, bleeding between periods, or postmenopausal bleeding.
.Pain During Urination or Intercourse: Pain or discomfort in the pelvic area may be present.
.Unexplained Weight Loss: Unexplained or sudden weight loss may also be a symptom of uterine cancer.
Treatment for uterine cancer depends on the stage of the cancer, the patient's health, and other factors. Common treatment options include:
.Surgery: The primary treatment for uterine cancer is surgery, which typically involves removing the uterus (hysterectomy). In some cases, the ovaries and fallopian tubes may also be removed.
.Radiation Therapy: High-energy radiation is used to target and destroy cancer cells. This can be used before or after surgery or as a standalone treatment.
.Chemotherapy: Drugs are used to kill cancer cells or stop their growth. Chemotherapy may be used if the cancer has spread to other areas.
Uterine cancer is a serious condition, but with early detection and appropriate treatment, many women can successfully recover and lead healthy lives. If you experience any symptoms or risk factors for uterine cancer, it is essential to seek medical advice as soon as possible for timely diagnosis and intervention. Remember that treatment options vary based on the cancer's stage and individual health conditions, and your healthcare provider will guide you through the best course of action.
Sonography (also known as ultrasound) is a non-invasive diagnostic imaging technique that uses high-frequency sound waves to create visual images of the internal organs and structures within the body. It is commonly used for a variety of medical purposes, including monitoring pregnancies, diagnosing diseases, and guiding treatments.
Sonography is typically recommended in the following situations:
.Pregnancy Monitoring: Sonography is essential for tracking the development of the fetus during pregnancy, checking for any complications, and monitoring the health of both mother and baby.
.Abdominal Pain: It helps diagnose the cause of unexplained abdominal pain, such as gallstones, kidney stones, or liver problems.
.Detecting Tumors or Cysts: Sonography is commonly used to detect tumors, cysts, or abnormalities in organs like the liver, kidneys, ovaries, and thyroid.
.Heart and Blood Vessel Issues: Sonography can be used to examine the heart and blood vessels for conditions like valve problems, blood clots, or aneurysms.
There are various types of sonography used for different purposes:
.Abdominal Sonography: Used to examine organs like the liver, kidneys, pancreas, and gallbladder to detect conditions like stones, cysts, or tumors.
.Pelvic Sonography: Primarily used for examining the reproductive organs in women, such as the uterus and ovaries, for conditions like cysts or tumors.
.Cardiac Sonography: Also known as an echocardiogram, used to assess the heart's structure and function, checking for heart valve problems, blood clots, and other heart-related issues.
The Non-Stress Test (N.S.T.) is a routine prenatal test that is used to measure the baby's heart rate in response to its movements. It is commonly performed in the later stages of pregnancy to assess the health of the fetus and to detect any potential complications such as fetal distress.
The Non-Stress Test is typically recommended in the following situations:
.High-Risk Pregnancies: For pregnancies that are considered high-risk due to conditions such as diabetes, hypertension, or previous complications.
.Post-term Pregnancy: To monitor the condition of the baby when the pregnancy goes beyond 40 weeks.
.Decreased Fetal Movement: If the mother reports reduced movement of the baby, the N.S.T. helps to assess the baby's well-being.
.Medical Conditions: If the mother has certain medical conditions such as gestational diabetes or pre-eclampsia, the test may be recommended.
The Non-Stress Test is an important tool in prenatal care, offering reassurance regarding the well-being of the fetus, especially in high-risk pregnancies. It provides valuable information that helps doctors and healthcare providers make informed decisions about the next steps in the pregnancy.

At Deshmukh Hospital, our plastic surgery team combines expertise and advanced techniques to enhance your appearance and confidence. We offer personalized, safe, and natural results through a range of cosmetic and reconstructive procedures.

At Deshmukh Hospital, we provide expert gynecological care for women at every stage of life, from routine exams to specialized treatments. Our compassionate team supports your health with personalized care for family planning and reproductive health.
30+ Available
35+ Available
100+
15+ Member
20K
At Our Deshmukh Hospital Marketing Agency, we excel at recognizing the specific needs and problems of specialists in these fields. We offer personalized strategies to help them succeed in their areas of expertise.
Delivering tomorrow’s Deshmukh Hospital for your family. View Doctors Availability

Providing reliable care with the highest safety standards.
Expert surgeons delivering advanced and precise care.
Dedicated staff available around the clock for your care.
Providing quality medicines to support your recovery.
Patients can expect to receive top-notch treatment for various medical conditions, including Uterine Prolapse. The hospital's team of professionals is highly skilled and well-versed in their respective domains.
Deshmukh Hospital offers comprehensive surgical services, including Abdominal. The hospital's team of surgeons is highly experienced and uses state-of-the-art equipment to perform surgeries.
Deshmukh Hospital provides comprehensive services to support patient health and well-being, including Ovarian Diseases, Vaginoplasty, Gynaecological Cancer Treatment. These services ensure a full spectrum of care for patients.
Almost all hospitals maintain high-level cleanliness to keep patients safe from any infection. For more information on the cleanliness maintained at Deshmukh Hospital, you can check the customer ratings and reviews or visit the hospital in person.
Yes, most hospitals provide ambulance services for transporting patients to the hospital and back. However, it is recommended to check with Deshmukh Hospital for further information on this.
You can make payment Via Cash, UPI, PhonePe, Paytm.
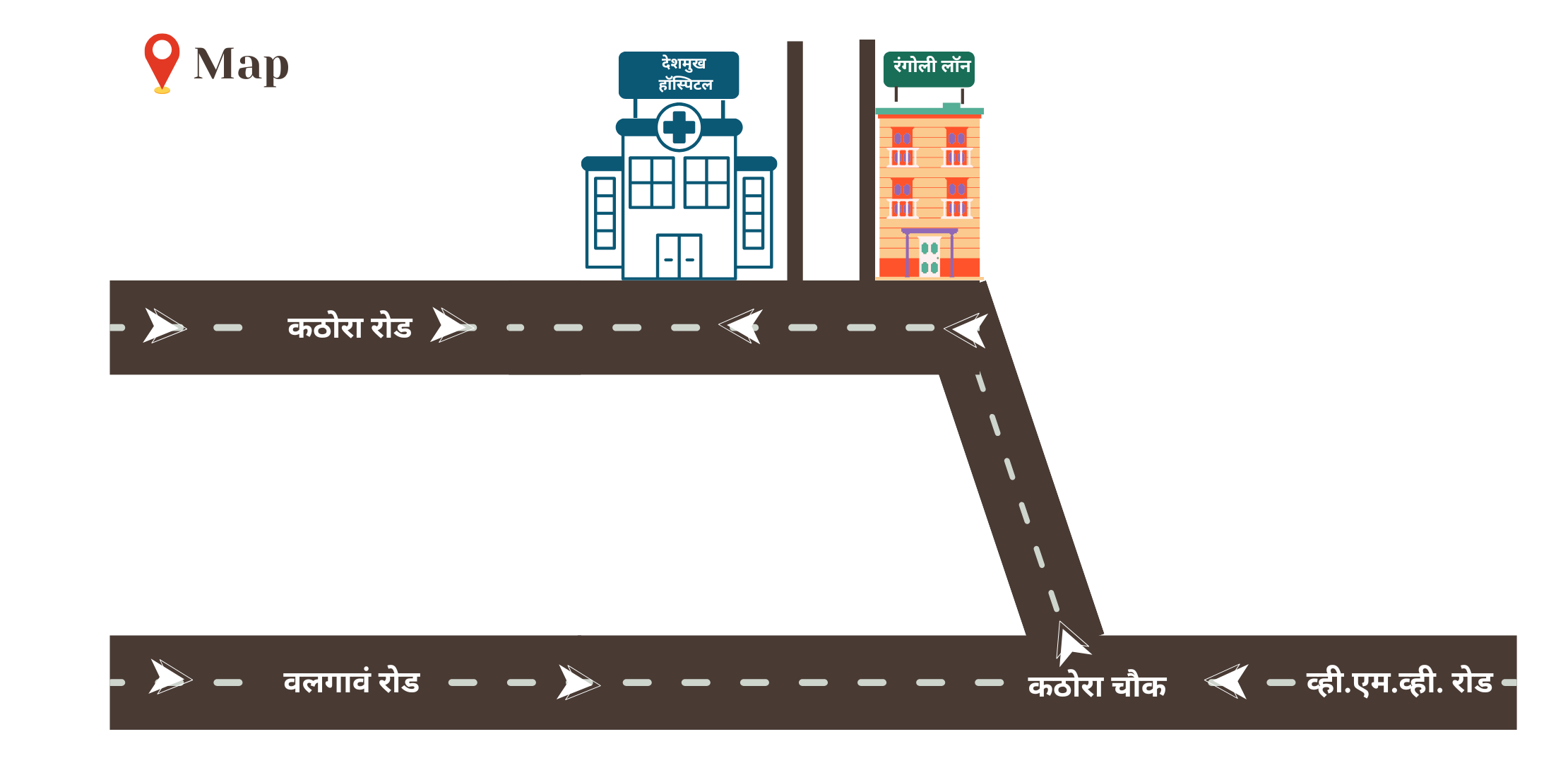
You can easily locate the establishment as it is in close proximity to Near Rangoli Lawn.
No, there are fixed visiting hours at hospitals. You can contact the Deshmukh Hospital for visiting hours.

© Copyright 2024- | All Rights Reserved | Terms & Conditions Apply.
How may I help you today?
Hello there! Need help? Reach out to us right here, and we'll get back to you as soon as we can!


